By Sarah Jane Tribble
CAIRO, Ga. — Zita Magloire fastidiously adjusted a comfortable measuring tape throughout Kenadie Evans’ pregnant stomach.
Figuring out a child’s dimension throughout a 28-week obstetrical go to is routine. However Magloire, a household doctor educated in obstetrics, is aware of that discovering the mom’s uterus and, thus, checking the infant, might be tough for inexperienced medical doctors.
“Generally it’s, like, off to the facet,” Magloire mentioned, displaying a visiting medical pupil find out how to press down firmly and full the hands-on examination. She moved her finger barely to calculate the fetus’s peak: “There she is, proper right here.”
Evans smiled and later mentioned Magloire made her “snug.”
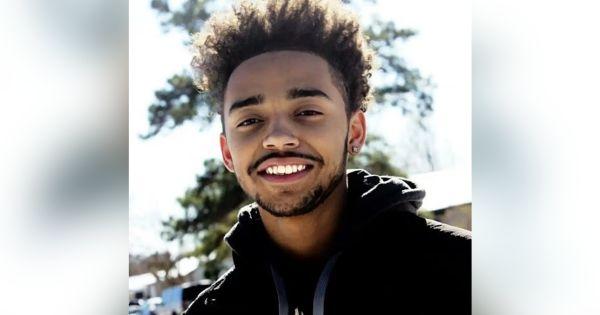
The 21-year-old had not too long ago relocated from Louisiana to southeastern Georgia, two states the place each maternal and toddler mortality are persistently excessive. She moved in together with her mom and grandfather close to Cairo, an agricultural neighborhood the place the hospital has a busy labor and supply unit. Magloire and different medical doctors on the native clinic the place she works ship lots of of infants there annually.
Scenes just like the one between Evans and Magloire recurrently play out on this rural nook of Georgia regardless of grim realities moms and infants face nationwide. Maternal deaths maintain rising, with Black and Indigenous moms most in danger; the variety of infants who died earlier than their 1st birthday climbed final 12 months; and greater than half of all rural counties in america don’t have any hospital companies for delivering infants, rising journey time for parents-to-be and inflicting declines in prenatal care.
There are a lot of causes labor and supply items shut, together with excessive working prices, declining populations, low Medicaid reimbursement charges, and staffing shortages. Household medication physicians nonetheless present the vast majority of labor and supply care in rural America, however few new medical doctors recruited to much less populated areas provide obstetrics care, partly as a result of they don’t need to be on name 24/7. Now, with rural America hemorrhaging well being care suppliers, the federal authorities is investing {dollars} and a spotlight to extend the ranks.
“Clearly the disaster is right here,” mentioned Hana Hinkle, government director of the Rural Coaching Observe Collaborative, which works with greater than 70 rural residency coaching packages. Federal grants have boosted coaching packages in recent times, Hinkle mentioned.

In July, the Division of Well being and Human Providers introduced an almost $11 million funding in new rural packages, together with household medication residencies that concentrate on obstetrical coaching.
Nationwide, a declining variety of main care medical doctors — inner and household medication — has made it tough for sufferers to ebook appointments and, in some instances, discover a physician in any respect. In rural America, coaching household medication medical doctors in obstetrics might be extra daunting due to low authorities reimbursement and rising medical legal responsibility prices, mentioned Hinkle, who can also be assistant dean of Rural Well being Professions on the College of Illinois School of Drugs in Rockford.
Within the Nineteen Eighties, about 43% of common household physicians who accomplished their residencies have been educated in obstetrics. In 2021, the American Academy of Household Physicians’ annual follow profile survey discovered that 15% of respondents had practiced obstetrics.
But household medical doctors, who additionally present the complete spectrum of main care companies, are “the spine of rural deliveries,” mentioned Julie Wooden, a physician and senior vp of analysis, science, and well being of the general public on the AAFP.
In a survey of 216 rural hospitals in 10 states, household follow medical doctors delivered infants in 67% of the hospitals, and at 27% of the hospitals they have been the one ones who delivered infants. The information counted infants delivered from 2013 to 2017. And, the authors discovered, if these household physicians hadn’t been there, many sufferers would have pushed a median of 86 miles round-trip for care.
Mark Deutchman, the report’s lead writer, mentioned he was “on name for 12 years” when he labored in a city of two,000 residents in rural Washington. Clarifying that he was exaggerating, Deutchman defined that he was one in every of simply two native medical doctors who carried out cesarean sections. He mentioned one of the simplest ways to make sure household physicians can bolster obstetric items is to ensure they work as a part of a workforce to stop burnout, quite than as solo do-it-all medical doctors of outdated.
There must be a core group of physicians, nurses, and a supportive hospital administration to share the workload “in order that anyone isn’t on name 12 months a 12 months,” mentioned Deutchman, who can also be affiliate dean for rural well being on the College of Colorado Anschutz Medical Campus Faculty of Drugs. The varsity’s School of Nursing acquired a $2 million federal grant this fall to coach midwives to work in rural areas of Colorado.
Nationwide, groups of suppliers are making certain rural obstetric items keep busy. In Lakin, Kansas, Drew Miller works with 5 different household physicians and a doctor assistant who has carried out an obstetrical fellowship. Collectively, they ship about 340 infants a 12 months, up from simply over 100 yearly when Miller first moved there in 2010. Phrase-of-mouth and two close by obstetric unit closures have elevated their deliveries. Miller mentioned he has seen buddies and companions “from surrounding communities cease delivering simply from sheer burnout.”
In Galesburg, Illinois, Annevay Conlee has watched 4 close by obstetric items shut since 2012, forcing some pregnant individuals to drive as much as an hour and a half for care. Conlee is a working towards household medication physician and medical director overseeing 4 rural areas with a workforce of OB-GYNs, household physicians, and a nurse-midwife. “There’s not the power to be on 24/7 name on your ladies to ship,” Conlee mentioned. “There must be a bit of extra concord when recruiting in to essentially assist a workforce of physicians and midwives.”
In Cairo, Magloire mentioned working towards obstetrics is “simply important care.” Actually, being pregnant care represents only a slice of her affected person visits on this Georgia city of about 10,000 individuals. On a current morning, Magloire’s sufferers included two pregnant individuals in addition to a teen involved about hip ache and an ecstatic 47-year-old who celebrated shedding weight.

Cairo Medical Care, an unbiased clinic located throughout the road from the 60-bed Archbold Grady hospital, is in a neighborhood finest recognized for its peanut crops and because the birthplace of baseball legend Jackie Robinson. The historic downtown has brick-accented streets and the oldest movie show in Georgia, and a nook of the library is devoted to native historical past.
The clinic’s six medical doctors, who’re a mixture of household medication practitioners, like Magloire, and obstetrician-gynecologists, pull in sufferers from the encompassing counties and collectively ship practically 300 infants on the hospital annually.
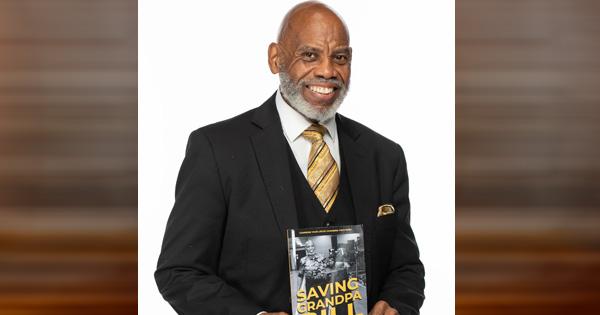
Deanna Buckins, a 36-year-old mom of 4 boys, mentioned she was relieved when she discovered “Dr. Z” as a result of she “utterly modified our lives.”
“She really listens to me and accepts my choices as an alternative of pushing issues upon me,” mentioned Buckins, as she held her 3-week-old son, whom Magloire had delivered. Years earlier, Magloire helped diagnose one in every of Buckins’ older youngsters with autism and constructed belief with the household.
“Say I am going in with one child; earlier than we go away, we’ve talked about each single child on how they’re doing and, you understand, getting caught up with life,” Buckins mentioned.
Magloire grew up in Tallahassee, Florida, and did her residency in rural Kansas. The smallness of Cairo, she mentioned, permits her to see sufferers as they develop — chatting up the youngsters when the moms or siblings come for appointments.
“She’s very pleasant,” Evans mentioned of Magloire. Evans, whose first baby was delivered by an OB-GYN, mentioned she was nervous about discovering the proper physician. The type of specialist her physician was didn’t matter as a lot as being with “somebody who cares,” she mentioned.
As a main care physician, Magloire can look after Evans and her youngsters for years to return.
KFF Well being Information is a nationwide newsroom that produces in-depth journalism about well being points and is without doubt one of the core working packages at KFF—an unbiased supply of well being coverage analysis, polling, and journalism. Be taught extra about KFF.