This publish was initially revealed on St. Louis American
By JoAnn Weaver
With the COVID-19 pandemic unwinding, a brand new health-related downside is unfolding.
In response to a report by Kaiser Household Basis (KFF), most Medicaid enrollees don’t know that states can resume disenrolling folks from Medicaid packages, like MO HealthNet. MO HealthNet presents well being care protection for eligible Missourians.
Steady enrollment in Medicaid ended on March 31, 2023, and over the approaching months, states will redetermine eligibility for folks enrolled in Medicaid and can disenroll those that are both now not eligible or who’re unable to finish the renewal course of, based on the KFF.
In response to a MO HealthNet report, the Division of Social Providers recognized 198,732 people who have been enrolled in Medicaid via MO HealthNet or have been answerable for a member of the family who was enrolled in MO HealthNet. 14.73% of the workforce of those corporations acquired MO HealthNet advantages for themselves or their households.
Roughly two-thirds (65%) of all Medicaid enrollees say they’re “unsure” if states are actually allowed to take away folks from Medicaid in the event that they now not meet the eligibility necessities or don’t full the renewal course of, with an extra 7% incorrectly saying states will not be allowed to do that, based on KFF.
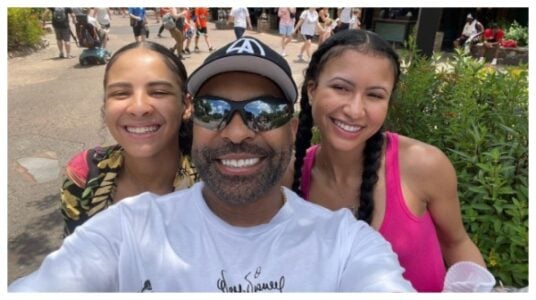
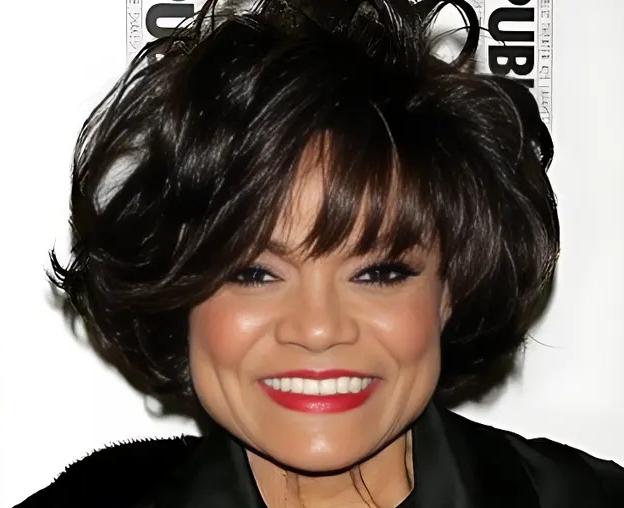
Nedra Bramlett-Stevenson, a volunteer with the American Most cancers Society Most cancers Motion Community and a Affected person Navigator at Barnes Jewish Hospital Breast Well being Middle, works with sufferers who might have their protection redetermined.
“All people doesn’t know that they’re enrolled in Medicaid, and that’s unhappy,” Bramlett-Stevenson stated. “They’ve this system now the place they’re attempting to make it possible for everybody, stays related to Medicaid, which suggests ensuring they replace their tackle, replace their cellphone quantity, however how can they do this they usually don’t know that they’re on Medicaid in the event that they’re not being notified via electronic mail letter, a cellphone name, a textual content message”
Almost half of Medicaid enrollees say they haven’t beforehand been via the Medicaid renewal course of, based on the Kaiser Household Basis.
“They’re not being notified by the federal government,” Bramlett-Stevenson stated. “I need to say the federal authorities is attempting to make it possible for all people stays enrolled, however it’s kinda exhausting as a result of once more, no one is aware of that they’ve been positioned on Medicaid till they might go to get a screening like a mammogram, or they might go to their major care doctor or any sort of specialty they usually say, ‘effectively, I don’t have insurance coverage.’”
One-third of Medicaid enrollees say they haven’t supplied up to date contact data to their state Medicaid company up to now 12 months,” based on KFF.
Medicaid started the method of creating positive that enrollees replace their cellphone quantity and tackle to maintain their insurance coverage in April earlier this 12 months. Stevenson desires to reiterate the significance of updating data to maintain Medicaid protection.
“We hear all this details about killing folks breaking into automobiles and all this different unfavourable stuff, however no one is speaking in regards to the Medicaid enlargement and how one can hold your Medicaid,” she stated. “No person is speaking about that, discuss to me in regards to the significance of sustaining steady protection, it’s essential as a result of for the reason that pandemic, all people has stopped getting their screenings, and now that every part is coming again up, all people must know it is rather essential so that you can go to your major care doctor.”
They want an advocate, healthcare supplier, or a healthcare particular person to assist them and push them to get again onto Medicaid.
nedra bramlett-stevenson, volunteer with the American Most cancers Society Most cancers Motion Community and Affected person Navigator at Barnes Jewish Hospital Breast Well being Middle
Whereas about six in ten of these with Medicaid as their solely supply of protection would search for protection from different sources in the event that they have been instructed they have been now not eligible, over 4 in ten say they wouldn’t know the place to search for different protection or can be uninsured, based on the Kaiser Household Basis (KFF).
“It’s essential that we get again to common screenings, like mammogram screenings, diabetes, prostate most cancers; all of the screenings are essential for, you recognize, that we’ve been getting earlier than the pandemic,” Bramlett-Stevenson stated.
In the course of the COVID-19 pandemic, states saved folks constantly enrolled in Medicaid in change for enhanced federal funding.
“They don’t know, and since it’s not being talked about,” the affected person navigator stated. “The one method it’s being talked about is as a result of you might have advocates that’s out right here going to totally different Federally-Certified Well being Facilities (FQHCs) and going to St. Louis County clinics and going to mom-and-pop retailers, and likewise going to the grocery shops handy out flyers.”
A majority of Medicaid enrollees say having knowledgeable assist with the renewal course of can be helpful, based on KFF. When requested what folks can do in the event that they lose their protection, Bramlett-Stevenson steered getting an knowledgeable or a affected person navigator like herself can help in getting the protection again.
“They want an advocate, healthcare supplier, or a healthcare particular person to assist them and push them to get again onto Medicaid,” she stated.
The American Most cancers Society Most cancers Motion Community volunteer went on to passionately speak about getting well being assets into the group so the uninsured can get the advantages outlined within the Medicaid Growth.
“We’re conscious of what assets we’ve right here in Missouri and no one is conscious of it, and once more, it’s since you get the gunshots and the killings and every part else overrides that, and that’s part of our group that’s failing,” Bramlett-Stevenson stated. “It’s having healthcare as a result of folks misplaced their jobs within the pandemic they usually don’t have any method of getting again the protection that they misplaced, so now that they’ve the Medicaid enlargement that’s on the market, they usually want a affected person navigator.”